Journal of Neurology, Neurological Science and Disorders
Impact of the COVID-19 pandemic on an Austrian population with or without pre-existing health issues
Stefanie Drach1*#, Emanuel Raphaelis1#, Patrick Langthaler1-3, Vanessa Frey1, Susanne Ring-Dimitriou4, Arne C Bathke2,3,5, Eugen Trinka1,6,7, Bernhard Iglseder8 and Bernhard Paulweber9
2Department of Artificial Intelligence and Human Interfaces, Paris Lodron University of Salzburg, Salzburg, Austria
3Team Biostatistics and Big Medical Data, IDA Lab Salzburg, Paris Lodron University of Salzburg and Paracelsus Medical University Salzburg, Salzburg, Austria
4Department of Sport and Exercise Science, Paris Lodron University of Salzburg, Salzburg, Austria
5Department of Statistics, University of Kentucky, Lexington, KY, USA
6Department of Public Health, Health Services Research and Health Technology Assessment, UMIT – University for Health Sciences, Medical Informatics and Technology, Hall in Tirol, Austria
7Neuroscience Institute, Christian Doppler University Hospital, Paracelsus Medical University and Centre for Cognitive Neuroscience, Salzburg, Austria
8Department of Geriatric Medicine, Christian Doppler University Hospital, Paracelsus Medical University, Salzburg, Austria
9Department of Internal Medicine, St. Johanns University Hospital, Private Medical University of Salzburg, Salzburg, Austria,
#contributed equally to this work
Cite this as
Drach S, Raphaelis E, Langthaler P, Frey V, Ring-Dimitriou S, et al. (2024) Impact of the COVID-19 pandemic on an Austrian population with or without pre-existing health issues. J Neurol Neurol Sci Disord 10(1): 027-038. DOI: 10.17352/jnnsd.000061Copyright
© 2024 Drach S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Background: The COVID-19 pandemic had significant effects on the well-being of individuals all over the world. The Austrian government decided to take various restrictions to contain the spread of the virus and thus protect the COVID-19 risk groups in particular. The aim of this study is to investigate how the COVID-19 risk groups perceive the pandemic and the restrictions to provide results for similar exceptional situations in the future.
Methods: For this purpose, we developed a questionnaire consisting of eleven items concerning the influence of the COVID-19 pandemic and the restrictions on well-being and behavior. Participants of the ongoing epidemiological Paracelsus 10,000 study (P10), in Salzburg, Austria, were included. We analyzed data from 989 people and classified the participants into three sub-groups depending on their risk of suffering from a severe course of a COVID-19 infection and tested for effects of risk group, sex, and their interaction. For a better overview we decided to group the questions into four main topics, named “changes in behavior and environment”, “worries caused by the virus and the restrictions”, “mood and mental state” and “long-lasting effects.”
Results: We found significant differences between the sub-groups in all main topics and a worsening in well-being across the entire sample. Especially anxiety, insecurity, nervousness, and sleep problems increased while satisfaction decreased.
Conclusion: The COVID-19 pandemic and the restrictions have created a highly uncertain environment and the topic was omnipresent and therefore had effects on the well-being and behavior of the risk groups as well as on our entire cohort.
Introduction
The year 2020 was overshadowed by the effects of a global Coronavirus disease (COVID-19) caused by an infection of SARS-CoV-2. The first cases of this virus infection in Austria were registered on February 25, 2020 [1]. On March 11, 2020, the World Health Organization declared COVID-19 a global pandemic [2]. People over 65 years of age and people with certain previous physical illnesses appeared to be particularly at risk for a severe course of COVID-19 [3]. In order to protect this risk group, the Austrian federal government ordered a nationwide lockdown as a measure to contain the spreading of the virus.
Brakemeier, et al. (2020) defined the COVID-19 pandemic as a new, unique, multidimensional, and potentially toxic stress factor with the following five specific characteristics: Global spread of unpredictable duration, individual effects on different areas of life, subjectively experienced loss of control, systemic effects on society, restrictions on healthcare facilities and protective factors such as leisure activities or sporting activity [4]. This makes the pandemic appear to be a particular threat to mental health [4-7].
Multiple review articles show the negative effects of the COVID-19-pandemic on well-being in the general population – especially higher scores of anxiety, depression, and stress [8-12] and also point out various risk factors like chronic physical illnesses for increasing psychological stress during the COVID-19-pandemic [8-15]. Kompaniyets and colleagues compared over 500,000 adults hospitalized with COVID-19 and found that anxiety disorders presented one of the strongest risk factors for severe COVID-19 illness [16].
A COVID-19 prevalence study from Austria published in November 2020 by the federal Austrian statistics bureau, Statistic Austria, examined the well-being of the Austrian population aged 16 and over. While 64% of the total population felt at least mostly in a good mood, restful, and relaxed, among the people with critical pre-existing illnesses only 33% did so [17].
The literature on the COVID-19 pandemic reveals negative effects on well-being both in the general population and in specific subgroups all over the world. With our Salzburg study, we contribute to the study landscape in Europe with regard to the impact of the COVID-19 pandemic. The aim of our study is to investigate how the COVID-19 risk groups perceive the pandemic and the restrictions to provide results for similar exceptional situations in the future.
We evaluated well-being and other areas of life in relation to the changed situation caused by COVID-19 and the consequential restrictions in a subsample (n = 989) of the Paracelsus 10,000 study (P10) conducted in Salzburg, Austria. The P10 is a prospective cohort study aiming to investigate the state of health among the inhabitants of Salzburg, Austria aged between 40 and 77 years. Between the years 2013 and 2020, 10,044 participants (f: 5,176, m: 4,868) were examined [18]. We divided the group into three sub-groups depending on their risk of suffering from a severe course of a COVID-19 infection. We assumed that there were differences between the risk groups in relation to the well-being and the behavior. For a better overview, we decided to group the questions into four main topics named “changes in behavior and environment”, “worries caused by the virus and the restrictions”, “moods and mental state”, and “long-lasting effects”.
Timeline of COVID-19 restrictions in Austria
- The 1st Lockdown determined by the Austrian government started on March 16 and covered the closedown of non-supply businesses, gastronomy, and schools. Meetings were prohibited and travel, as well as, 24-hour exit restrictions were imposed.
- The restrictions gradually eased from mid-April. Some businesses and federal gardens reopened.
- The restrictions were tightened again from September 22. Austria-wide mask requirements in publicly accessible indoor areas were imposed, as well as stricter regulations for events and gastronomy.
- From October 25 a maximum of 6 people + 6 children for private indoor meetings and 12 people outdoors were permitted to gather. One meter minimum distance outdoors, oral and nose cover also on train platforms.
- The lockdown light began on November 3 with exit restrictions from 8 p.m. to 6 a.m., temporary gastronomy and hotel business, leisure and cultural establishment closures, high schools on distance learning, etc.). Essential shops remained open.
- The 2nd lockdown was imposed from November 17 until December 6 with the same restrictions as the 1st lockdown.
- The questionnaires analyzed in this article were completed from October 12, 2020, to December 6, 2020, thus during a phase of continuous tightening of restrictive measures Figure 1.
Methods
Participants
For this investigation, participants of the P10 were asked to complete an online questionnaire. Due to time pressure and relevance of the topic we selected the participants out of the P10-cohort who had provided a valid e-mail address. All participants responded to the pseudo-anonymous survey and signed an informed consent form that was approved by the local ethics committee (415-E/1521/3-2012). In close reference to the definition of Austrian legal regulation for COVID-19 risk groups [3] and a meta-analysis by Ssentongo, et al. regarding pre-existing comorbidities and COVID-19 mortality [19], the following risk factors for a severe course of COVID-19 were defined for our analysis: age > 65, BMI > 30, current smoker, history of stroke, coronary heart disease, heart failure, hypertension, cancer, asthma, chronic obstructive pulmonary disease, cirrhosis, chronic hepatitis, diabetes and taking an antidiabetic drug. We classified the sample into three groups, with a presumed increasing risk of mortality from COVID-19 depending on the number of risk factors. Low risk was defined as having no risk factor, medium risk as having one, and high risk as having more than one risk factor. We did not quantify in more detail the additional risk caused by each individual risk factor.
Data collection
The data of the questionnaire were collected via an online questionnaire. We used the software EvaSys to collect participants’ responses. Even though the program is internet-based, it was incorporated into the internal hospital IT system, protected by the relevant firewall. We developed an 11-item questionnaire partly adapted from standardized questionnaires [20,21], focusing on changes in well-being and behavior at the beginning of the COVID-19 pandemic and the following restrictions. The questionnaire addresses concerns regarding the impact of the disease and the restrictions on health, well-being, family situation, financial situation, medical facilities, feelings, and conditions since the beginning of the COVID-19 pandemic compared to before. The questionnaire contains several response options formats in the form of a Likert scale, multiple answers, and binary answers. The first question is based on Dalbert`s “Mood level scale” [20] and Kessler`s psychological distress scale [21] and was adapted to our questionnaire. Questions two – eleven were self-developed Table 1 shows the eleven questions, the answer format, and the development of the respective question.
For classifying the participants into the risk subgroups (low, medium, high), we used data collected by the P10 (The information about the history of diseases was collected via a face-to-face interview, the BMI was calculated from height and weight measurements, and the smoking habit was determined from self-reports).
For question 1 an ordinal sum score was created by coding “less” as -1, “more” as 1, and “the same” and “no answer” as 0 (variables asking for positive mood states were coded in reverse) and summing up the answers to all the variables. For question 2 a logistic regression model was fitted for the probability of answering “yes”. For the sub-question of question 3 regarding the fear of negative financial effects participants who were retired or unemployed at the start of the pandemic were excluded. For question 4 activities were grouped into leisurely (shopping, restaurants, churches, cultural, cinemas, playground, sport, events, travel) and non-leisurely (all remaining categories) activities, and a sum score was created for each category coding the possible answers from 0 to 3. For question 5, people who were retired or unemployed at the start of the pandemic were excluded, resulting in a binary variable. For question 6 all categories starting with yes were joined into one category and people who did not want to answer were excluded, resulting in a binary variable. For question 7 a logistic regression model was fitted for the probability of checking each box separately. For questions 8 and 9 participants who did not drink/smoke were excluded and the remaining possible answers (less, same, more) were interpreted as an ordinal variable. For question 10 a multinomial regression model was fitted with “neither” as the reference category. For question 11 a logistic regression model was fitted for each possible answer.
Statistical analyses
All statistical analyses were conducted using the software environment R [22]. For each analyzed outcome, we tested for an influence of risk group (low-, medium-, high-RG), sex (female, male), and the interaction of the two. For binary outcomes, logistic regression was used. For ordinal outcomes, we used a nonparametric ANOVA-type test [23,24] for the equality of the relative treatment effect (RTE) implemented in the R package rankFD [25]. In the case of significant effects, post-hoc tests for appropriate contrasts were conducted. For the logistic regression models, the package multcomp [26] was used, for the nonparametric models an ANOVA-type test for the appropriate contrast was computed. Due to the exploratory nature of the study, we did not adjust for multiple comparisons.
Results
Participant description
For this investigation, 3,033 participants of the P10 were asked to complete a COVID-19 questionnaire. The number of returned questionnaires was 1,150. We had to exclude 161 of the returned questionnaires from analysis due to incomplete answers or as it was not possible to determine their risk group. In total, we were able to analyze 989 questionnaires from participants aged between 43 and 75 years (Mean = 57.14, SD = 7.72), 388 women and 601 men.
See Table 2 for the frequency of the individual risk factors (Participants with more than one risk factor are counted once in each corresponding category) and Table 3 for a breakdown of the sample by sex and risk groups.
Questions
Changes in behavior and environment: Participants were asked if they had to be in quarantine at some point during the first year of the pandemic. Sixty-seven participants answered with “yes”, and 905 participants with “no”. There was a significant effect for the risk group. Participants in the high-risk group had significantly lower odds of being in quarantine than participants in the low-risk group (OR = 0.33, 95% CI: (0.11, 0.98), z = -1.997, p = .046). There was no significant sex or interaction effect on the probability of being in quarantine. There was no significant difference between the medium vs. low-risk group (OR = 0.78, 95% CI: (0.44, 1.37), z = -0.862, p = .389) and the high vs. medium-risk group (OR = 0.42, 95% CI: (0.13, 1.31), z = -1.497, p = .134) (Figure 2A).
Two hundred fifty-nine participants stated that they were restrained from visiting a medical facility, while 652 participants were not. There was no significant risk group, sex, or interaction effect on the probability of being restrained from visiting a medical facility (Figure 2B).
Of the 739 participants who had employment before the lockdown, 507 reported that their work environment changed, whereas 232 reported that it did not change. There was no significant risk group, sex, or interaction effect on the probability of the work environment changing (Figure 2C).
One hundred sixty-one participants reported not drinking any alcohol. Of the ones that did report drinking alcohol, 87 reported an increase in consumption, 604 reported no change and 136 reported a decrease since the beginning of the pandemic. Among people consuming alcohol there was no significant risk group, sex, or interaction effect on the change in alcohol consumption since the beginning of the pandemic (Figure 2D).
Eight hundred thirty participants reported not smoking. Of the ones that did report smoking, 26 reported an increase in consumption, 107 reported no change and 20 reported a decrease since the beginning of the pandemic. Among people who smoked there was no significant risk group, sex, or interaction effect on the change in smoking habit since the beginning of the pandemic (Figure 2E).
Nine hundred seventy participants responded to deal more with at least one activity of question 7 during the pandemic. Subjects in the low-risk group were significantly more likely to do sports than subjects in the medium (OR = 1.49, 95% CI: (1.10, 2.01), z = 2.546, p = .011) and high (OR = 2.24, 95% CI: (1.51, 3.30), z = 4.044, p < .001) risk group. Subjects in the high-risk group were significantly more likely to watch TV than subjects in the low (OR = 1.66, 95% CI: (1.17, 2.37), z = 2.829, p = .005) but not in the medium (OR = 1.17, 95% CI: (0.80, 1.70), z = 0.820, p = .412) risk group. Subjects in the medium-risk group were significantly more likely to watch TV than subjects in the low-risk group (OR = 1.42, 95% CI: (1.06, 1.92), z = 2.332, p = .020). Subjects in the low-risk group were significantly more likely to spend time with the family than subjects in the high (OR = 1.86, 95% CI: (1.25, 2.77), z = 3.054, p = .002) risk group. Subjects in the medium-risk group were significantly more likely to spend time with family than subjects in the high-risk group (OR = 1.81, 95% CI: (1.19, 2.75), z = 2.775, p = .006). Subjects in the low-risk group were significantly more likely to meditate than subjects in the high (OR = 2.84, 95% CI: (1.32, 6.14), z = 2.663, p = .008) (Figure 3).
Women were significantly more likely to read (OR = 3.40, 95% CI: (2.52, 4.58), z = 8.001, p < .001), cook (OR = 3.35, 95% CI: (2.51, 4.48), z = 8.190, p < .001), clean (OR = 2.09, 95% CI: (1.57, 2.78), z = 5.034, p < .001), meditate (OR = 2.56, 95% CI: (1.44, 4.55), z = 3.201, p = .001) and paint (OR = 2.36, 95% CI: (1.06, 5.26), z = 2.219, p = .035) than men. Men were significantly more likely to spend time using electronic devices (OR = 1.79, 95% CI: (1.35, 2.38), z = 4.034, p < .001), do sports (OR = 1.62, 95% CI: (1.19, 2.20), z = 3.098, p = .002) and spend time with their family (OR = 1.45, 95% CI: (1.06, 1.97), z = 2.361, p = .018) than women (Figure 3).
For chi-squared values, degrees of freedom, and p-values of risk group, sex, and interaction of risk group and sex regarding question 7 (supplementary information).
Worries caused by the virus and the restrictions
Nine hundred eighty-nine participants responded to the question about the “fear of contracting the virus” and “fear of a negative effect on family life”, and 739 participants responded to “fear of the financial situation” and “fear of unemployment”. There was a significant effect of sex, with women reporting lower levels of “fear of contracting the virus (ΔRTE = - 0.039, 95% CI: (-0.075, -0.003), z = -2.134, p = .033) than men (Figure 4B). There were no significant effects between the risk groups, sex, or their interaction regarding “fear of contracting the virus” (Figure 4A), “fear of a negative effect on family life” (Figure 4B), “fear of the financial situation” (Figure 4C), “fear of unemployment” (Figure 4D).
Nine hundred and sixty participants responded to the question of whether health, society, economy, or restrictions of freedom by the lockdown preoccupied them the most. There was a significant risk group effect on the probability of choosing health-related consequences as an answer. Participants in the high-risk group had significantly higher odds of choosing health-related consequences as an answer than participants in the medium (OR = 1.72, 95% CI: (1.17, 2.54), z = 2.735, p = .006) and low (OR = 1.94, 95% CI: (1.34, 2.80), z = 3.538, p < .001) risk group. There was no significant difference in the medium vs. low-risk group (OR = 1.13, 95% CI: (0.84, 1.51), z = 0.788, p = .431) There was no significant effect between the risk groups, sex, or their interaction for choosing the topics society and economy and restrictions of freedom. There was no significant sex or interaction effect on the probability of choosing health-related consequences as an answer. (Figure 5).
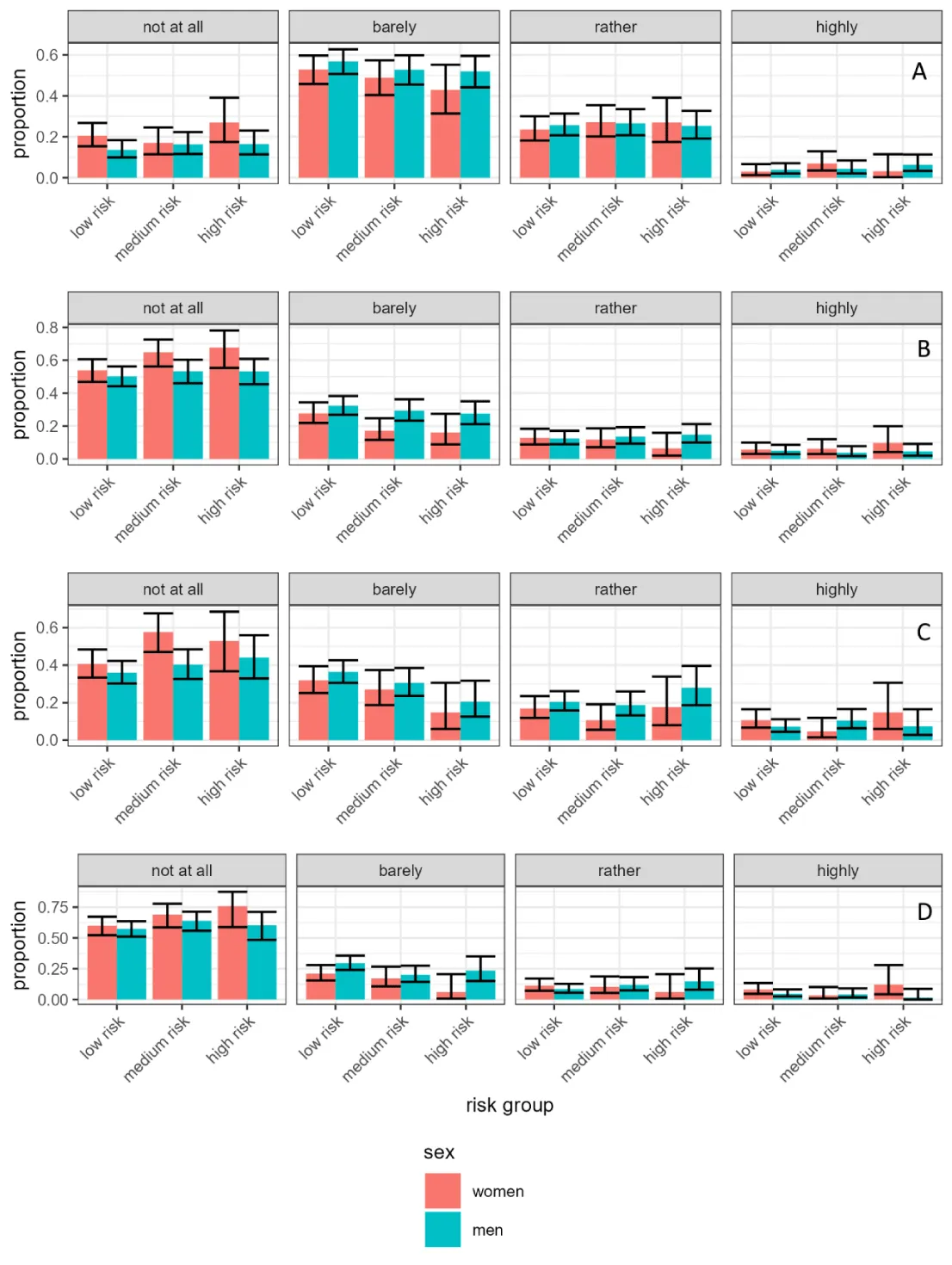
Mood and mental state
Among the 935 participants providing answers regarding changes in different moods and mental states, there was a tendency to report worse mood during the pandemic than before as indicated by the median being above zero (Median = 1, CI: (1, 2), p < .001, binomial test). The percentage of participants reporting a score above zero ranged from 51.2% for women in the medium-risk group to 61.0% for men in the low-risk group. In the whole sample, 56.4% of participants reported a worsening of mood. There was no significant risk group, sex, or interaction effect on the sum score of mood and mental state (Figure 6A).
Among the 952 participants providing answers regarding a negative effect on mood due to restrictions on leisurely activities, there was no significant risk group, sex, or interaction effect on the effect of the restrictions on mood (Figure 6B).
Among the 873 participants providing answers regarding a negative effect on mood due to restrictions on non-leisurely activities, there was a significant effect on the risk group. Participants in the medium-risk group reported significantly lower negative effects on mood than participants in the low-risk group (ΔRTE = -0.067, 95% CI: (-0.112, -0.021), z= -2.907, p = .004). There was no significant difference between the high vs. low-risk groups (ΔRTE = -0.036, 95% CI: (-0.089, 0.017), z = -1.346, p = .178) or the high vs. medium-risk groups (ΔRTE = 0.031, 95% CI: (-0.027, 0.088), z = 1.050, p = .294) There was no significant sex or interaction effect on the effect of the restrictions on mood. (Figure 6C).
Long-lasting effects
Among the participants providing answers about the long-lasting effects of the curfew, 58 reported positive effects, 79 reported negative effects, 233 reported positive and negative effects, and 614 reported neither. Using “neither” as the reference category, there was a significant effect of the risk group on the probability of choosing “positive” over “neither”. Participants in the high-risk group had significantly lower odds of choosing “positive” over “neither” than participants in the medium-risk group (OR = 0.41, 95% CI: (0.18, 0.96), z = -2.05, p = .040). Participants in the medium-risk group had significantly higher odds of choosing “positive” over “neither” than participants in the low-risk group (OR = 1.81, 95% CI: (1.00, 3.26, p = .049)). There was no significant difference in the high vs. low-risk group (OR = 0.75, 95% CI: (0.32, 1.76), z = -0.66, p = .507) There was no significant effect of risk group, sex, or interaction on the probability of choosing “both” over “neither” and “negative” over “neither”. There was no significant effect of sex or interaction of sex and risk group on the probability of choosing “positive” over, or “neither” (Figure 6D).
For raw data, statistics, and p-values of the risk group, sex, and interaction for all questions (except question 7) of the questionnaire (Supplementary information).
Discussion
In this study during the second lockdown in Salzburg, Austria, we could identify a major impact on well-being without a significant difference between the risk groups. Over the whole sample, we can see a reduction in well-being, including anxiety, stress, and sleep problems in 30% - 50% of the cases. This result aligns with numerous other studies that have observed a decline in mood, particularly in terms of symptoms of depression, anxiety, and sleep disorders [27-29]. One of these studies looked at data from 204 countries, so this is a global phenomenon and the results from our study underpin these significant psychological effects [27].
Lockdowns during the COVID-19 pandemic are a burden to well-being for several reasons. The limited interpersonal exchange can lead to feelings of loneliness and isolation [30]. The widespread economic disruptions can cause job losses or other financial insecurities resulting in financial stress [30,31]. Fears of contracting COVID-19 can be detrimental to well-being as well as a lack of structure in daily activities caused by the lockdowns. The exposure of individuals to traumatic physical or psychological events is naturally higher during a pandemic [27-30].
Subpopulations with a low, medium, or high risk for severe illness with respect to a COVID-19 infection (risk factors age > 65, BMI > 30, history of stroke, coronary heart disease, heart failure, hypertension, cancer, asthma, chronic obstructive pulmonary disease, cirrhosis, chronic hepatitis, diabetes) were assessed and compared. In line with these burdens, the results show a worsening of well-being across all groups during the COVID-19 pandemic, regardless of underlying health conditions. They show comparable scores for all risk groups with respect to well-being. Differences between men and women are negligible. A possible explanation would be that the pandemic has created a highly uncertain and challenging environment that has affected everyone, regardless of their preexisting health status. It is also possible that individuals with preexisting health conditions may have developed coping mechanisms to manage the added stress or have access to support, e.g. in the form of psychotherapy or medication through a more regular contact with a healthcare provider. Additionally, studies show that individuals directly affected by stressful events often exhibit less fear compared to those not directly affected (the paradox of subjective well-being) [32]. Another approach is that some individuals in the risk group may have underestimated their risk due to conscious or unconscious ignorance of their health condition, therefore there could possibly exist a bias in reporting the subject phenomenon. This possibility is only partially backed by the results, as the high-risk group was on the one hand significantly more occupied with health-related consequences of the pandemic, but on the other hand was not more worried about contracting the virus. A possible interpretation would be that these were in part greater worries of not getting adequate medical treatment for health conditions different than a COVID-19 infection, due to restricted free capacities in hospitals.
There was a significant main effect for sex and worry about family life, with women being less worried about family life overall. It is possible that there are different coping strategies in men and women, with women seeking more support from family or friends or engaging in helping self-care activities, while men are more likely to internalize worries and emotions, leading to greater levels of stress. Women were significantly more likely to read, cook, clean, meditate, and paint than men. Men were significantly more likely to spend time using electronic devices, do sports, and spend time with their families than women.
Yet, this would be in contrast to existing literature showing that across cohorts, higher prevalence rates of internalizing disorders were found for women [33]. More research is needed to see if this applies to the mental health burdens in the COVID-19 pandemic as well. These findings suggest a complex interplay between gender, coping strategies, and mental health outcomes, highlighting the importance of considering multiple factors for a better understanding of mental health disparities between genders.
In terms of lifestyle and recreational activities, notable distinctions were observed among different risk groups. The low-risk group shows a significantly higher likelihood of engaging in sports compared to both the middle and high-risk groups. Conversely, the high-risk group demonstrated a greater inclination towards watching television when compared to the low-risk group, with the middle-risk group being in between.
Regarding social activities, the low-risk group was significantly more inclined to spend time with family than the high-risk group. Similarly, the middle-risk group surpassed the high-risk group in the likelihood of spending time with family. These findings suggest that lifestyle and recreational activities are valid indicators of risk profiles, with engagement in physical activity potentially contributing to lower risk levels, while sedentary behaviours like television watching may correlate with higher risk profiles. Furthermore, in practices related to mental well-being, the low-risk group showed a significantly higher propensity for meditation compared to the high-risk group. These lifestyle differences among risk groups highlight varied coping mechanisms and recreational preferences among the different risk groups during the challenges posed by the COVID-19 pandemic. This suggests that engagement in activities like meditation or sports may influence an individual’s risk profile for mental health challenges during the COVID-19 pandemic. However, it’s important to note that while these associations suggest a potential influence of lifestyle on risk, establishing causality would require further research, to determine if changes in lifestyle directly affect risk levels or if they are merely correlated.
In relation to the influence of the exit restrictions on current life, the high-risk group had significantly lower odds of choosing “positive influence” over “neither influence” than the middle-risk group. The middle-risk group had significantly higher odds of choosing “positive influence” over “neither influence” than the low-risk group. This suggests that the impact of exit restrictions on individuals’ lives varies depending on their risk group. Specifically, the high-risk group is less likely to perceive exit restrictions as positively influencing their lives compared to the middle-risk and low-risk groups. These findings highlight the differential experiences and perspectives on exit restrictions among different risk groups. It may seem counterintuitive or even paradoxical that the high-risk group, which could benefit more from protective measures like exit restrictions, is less likely to perceive them positively compared to the middle-risk and lower-risk groups. This could be due to several factors, such as the perceived burden of restrictions on daily life, mental health impacts, or individual interpretations of risk and protection.
Limitations
Please note that the discussed results are not familywise type I error-controlled. Another limitation is the development of our questionnaire which we created a few months after the outbreak of the pandemic. At that time we were not aware of a standardized COVID-19 inventory so we developed a questionnaire partly based on proven standardized surveys and adapted it to the Austrian situation and our subjects. The disproportion between women and men should also be mentioned. Furthermore, limitations regarding the self-reported information on morbidities and the response to our questionnaire, like honest answers, language barrier, and understanding of questions, must be taken into account. A past COVID-19 infection or one that existed at the time the questionnaire was filled out could also have a potential impact on the questionnaire results.
Conclusion and main findings
Comparative analysis of risk groups
The study compares subpopulations with varying risk levels for severe COVID-19 infection. It contributes by showing that regardless of risk factors, there was a decline in well-being across all groups. The most likely explanation is that the pandemic has created a highly uncertain and challenging environment that has affected everyone, regardless of their preexisting health status. In addition, it supports the idea of effective and well-functioning access to psychological and medical support systems in the region of Salzburg, Austria.
Risk-group specific coping mechanisms and worries
Notable differences in coping strategies and recreational activities were observed among different risk groups, highlighting the diverse responses to pandemic-related challenges.
Gender-specific coping mechanisms and worries
The study highlights potential gender-specific coping strategies and worries during the pandemic, shedding light on how men and women may respond differently to stressors and showing women being less worried about family life during the pandemic and men showing unexpectedly higher tendencies to internalize worries and emotions.
Outlook
Further research is needed to evaluate if there are even more specific subpopulations with preexisting conditions that may be especially vulnerable to well-being challenges related to the pandemic.
Drawing comparisons with previous pandemics (e.g., H1N1, SARS) could provide insights into how different types of pandemics impact well-being and whether there are lessons that can be applied in future public health crises.
While this study focused on the second lockdown, it would be valuable to conduct follow-up studies to understand the long-term effects on well-being. This could help identify individuals or subpopulations that may show resilience or those who may continue to struggle.
Statement of ethics
All participants signed an informed consent and the study protocol was approved by the ethics committee of the country of Salzburg (415-E/1521/3-2012).
Disclosure statement
Eugen Trinka has received consultancy fees from Arvelle Therapeutics, Argenx, Clexio, Celegene, UCB Pharma, Eisai, Epilog, Bial, Medtronic, Everpharma, Biogen, Takeda, Liva-Nova, Newbridge, Sunovion, GW Pharmaceuticals, and Marinus; speaker fees from Arvelle Therapeutics, Bial, Biogen, Böhringer Ingelheim, Eisai, Everpharma, GSK, GW Pharmaceuticals, Hikma, Liva-Nova, Newbridge, Novartis, Sanofi, Sandoz and UCB Pharma; research funding (directly, or to his institution) from GSK, Biogen, Eisai, Novartis, Red Bull, Bayer, and UCB Pharma outside the submitted work. Eugen Trinka receives Grants from the Austrian Science Fund (FWF), Österreichische Nationalbank, and the European Union. Eugen Trinka is the CEO of Neuroconsult Ges.m.b.H.
Authors contributors
The authors thank all contributors of the study, particularly: Alison Barnewald. We especially express our gratitude to the participants of the Paracelsus 10,000 study.
- World Health Organization. WHO – COVID-19 dashboard [Internet]. 2020 Feb [cited 2023 Oct 25]. https://data.who.int/dashboards/covid19/cases?m49=040&n=c
- WHO Director-General. Opening remarks at the media briefing on COVID19 [Internet]. 2020 Mar [cited 2023 Oct 28]. https://scholar.google.com/scholar?q=WHO+Director.General%E2%80%99s+opening+remarks+at+the+Media+briefing+on+COVID19±March+2020+
- Entire legal provision for the COVID-19 risk group regulation. Federal legal information system. 2020MayGesamte Rechtsvorschrift für COVID-19-Risikogruppe-Verordnung. 2020. https://www.ris.bka.gv.at/GeltendeFassung.wxe?Abfrage=Bundesnormen&Gesetzesnummer=20011167
- Brakemeier EL, Wirkner J, Knaevelsrud C, Wurm S, Christiansen H. The COVID-19 pandemic as a mental health challenge. Journal of Clinical Psychology and Psychotherapy. 2020; 49(1): 1-31. doi.org/10.1026/1616-3443/a000574
- Oblath R, Dayal R, Loubeau JK, Lejeune J, Sikov J, Savage M, Posse C, Jain S, Zolli N, Baul TD, Ladino V, Ji C, Kabrt J, Sidky L, Rabin M, Kim DY, Kobayashi I, Murphy JM, Garg A, Spencer AE. Trajectories and correlates of mental health among urban, school-age children during the COVID-19 pandemic: a longitudinal study. Child Adolesc Psychiatry Ment Health. 2024 Mar 14;18(1):32. doi: 10.1186/s13034-024-00712-4. PMID: 38486248; PMCID: PMC10941406.
- Kupcova I, Danisovic L, Klein M, Harsanyi S. Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychol. 2023 Apr 11;11(1):108. doi: 10.1186/s40359-023-01130-5. PMID: 37041568; PMCID: PMC10088605.
- World Health Organization. Mental Health and COVID-19: Early evidence of the pandemic’s impact 2022 Mar https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1
- Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun. 2020 Oct;89:531-542. doi: 10.1016/j.bbi.2020.05.048. Epub 2020 May 30. PMID: 32485289; PMCID: PMC7260522.
- Santabárbara J, Lasheras I, Lipnicki DM, Bueno-Notivol J, Pérez-Moreno M, López-Antón R, De la Cámara C, Lobo A, Gracia-García P. Prevalence of anxiety in the COVID-19 pandemic: An updated meta-analysis of community-based studies. Prog Neuropsychopharmacol Biol Psychiatry. 2021 Jul 13;109:110207. doi: 10.1016/j.pnpbp.2020.110207. Epub 2020 Dec 15. PMID: 33338558; PMCID: PMC7834650.
- Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, Rasoulpoor S, Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020 Jul 6;16(1):57. doi: 10.1186/s12992-020-00589-w. PMID: 32631403; PMCID: PMC7338126.
- Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, McIntyre RS. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020 Dec 1;277:55-64. doi: 10.1016/j.jad.2020.08.001. Epub 2020 Aug 8. PMID: 32799105; PMCID: PMC7413844.
- Chan VKY, Chai Y, Chan SSM, Luo H, Jit M, Knapp M, Bishai DM, Ni MY, Wong ICK, Li X. Impact of COVID-19 pandemic on depression incidence and healthcare service use among patients with depression: an interrupted time-series analysis from a 9-year population-based study. BMC Med. 2024 Apr 22;22(1):169. doi: 10.1186/s12916-024-03386-z. PMID: 38644506; PMCID: PMC11034087.
- Asadi-Pooya AA, Trinka E, Hingray C, Fawaz A, Karakis I, Kishk NA, Farazdaghi M, Höfler J, Tarrada A, Ashkanani A, Risman A, Rizk H. An international study of the effects of the COVID-19 pandemic on characteristics of functional seizures. Epilepsy Behav. 2022 Feb;127:108530. doi: 10.1016/j.yebeh.2021.108530. Epub 2021 Dec 29. PMID: 35016054; PMCID: PMC8714296.
- Volkers N, Wiebe S, Asadi-Pooya AA, Balagura G, Gómez-Iglesias P, Guekht A, Hall J, Ikeda A, Jetté N, Kishk NA, Murphy P, Perucca E, Pérez-Poveda JC, Sanya EO, Trinka E, Zhou D, Cross JH. The initial impact of the SARS-CoV-2 pandemic on epilepsy research. Epilepsia Open. 2021 Jun;6(2):255-265. doi: 10.1002/epi4.12471. Epub 2021 Feb 26. PMID: 34033250; PMCID: PMC8013398.
- Cross JH, Kwon CS, Asadi-Pooya AA, Balagura G, Gómez-Iglesias P, Guekht A, Hall J, Ikeda A, Kishk NA, Murphy P, Kissani N, Naji Y, Perucca E, Pérez-Poveda JC, Sanya EO, Trinka E, Zhou D, Wiebe S, Jette N; ILAE Task Forces on COVID-19, Telemedicine. Epilepsy care during the COVID-19 pandemic. Epilepsia. 2021 Oct;62(10):2322-2332. doi: 10.1111/epi.17045. Epub 2021 Aug 24. PMID: 34428314; PMCID: PMC8652685.
- Kompaniyets L, Pennington AF, Goodman AB, Rosenblum HG, Belay B, Ko JY, Chevinsky JR, Schieber LZ, Summers AD, Lavery AM, Preston LE, Danielson ML, Cui Z, Namulanda G, Yusuf H, Mac Kenzie WR, Wong KK, Baggs J, Boehmer TK, Gundlapalli AV. Underlying Medical Conditions and Severe Illness Among 540,667 Adults Hospitalized With COVID-19, March 2020-March 2021. Prev Chronic Dis. 2021 Jul 1;18:E66. doi: 10.5888/pcd18.210123. PMID: 34197283; PMCID: PMC8269743.
- Paškvan M, Kowarik A, Schrittwieser K, Till, M, Weinauer M. COVID-19 Prevalence April 2020 – Results Report. Statistics Austria – Federal Ministry of Education. Science and Research. 2020; 27-29. https://www.statistik.at/fileadmin/pages/1693/COVID
- Frey V, Langthaler P, Raphaelis E, Ring-Dimitriou S, Kedenko L, Paracelsus 10,000: An Observational Cohort Study about the Health Status of the Population of Salzburg, Austria. Rationale, Objectives and Study Design. Paracelsus Proceedings of Experimental Medicin. 2023; 1:1-17.
- Ssentongo P, Ssentongo AE, Heilbrunn ES, Ba DM, Chinchilli VM. Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis. PLoS One. 2020 Aug 26;15(8):e0238215. doi: 10.1371/journal.pone.0238215. PMID: 32845926; PMCID: PMC7449476.
- Dalbert C. Subjective Well-being of Young Adults: Theoretical and Empirical Analysis of Structure and Stability: Journal of Differential and Diagnostic Psychology. 1992; 13:207-220.
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002 Aug;32(6):959-76. doi: 10.1017/s0033291702006074. PMID: 12214795.
- R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria 2022; https://www.R-project.org/.
- Brunner E, Dette H, Munk A. Box-Type Approximations in Nonparametric Factorial Designs. Journal of the American Statistical Association. 1997; 92:1494-1502.
- Brunner E, Bathke AC, Konietschke F. Rank and Pseudo-Rank Procedures for Independent Observations in Factorial Designs. Springer International Publishing. 2018.
- Konietschke F, Friedrich S, Brunner E, Pauly M. _rankFD: Rank-Based Tests for General Factorial Designs_. R package version 0.1.1. 2022; https://CRAN.R-project.org/package=rankFD.
- Hothorn T, Bretz F, Westfall P. Simultaneous inference in general parametric models. Biom J. 2008 Jun;50(3):346-63. doi: 10.1002/bimj.200810425. PMID: 18481363.
- COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021 Nov 6;398(10312):1700-1712. doi: 10.1016/S0140-6736(21)02143-7. Epub 2021 Oct 8. PMID: 34634250; PMCID: PMC8500697.
- Tsamakis K, Triantafyllis AS, Tsiptsios D, Spartalis E, Mueller C, Tsamakis C, Chaidou S, Spandidos DA, Fotis L, Economou M, Rizos E. COVID-19 related stress exacerbates common physical and mental pathologies and affects treatment (Review). Exp Ther Med. 2020 Jul;20(1):159-162. doi: 10.3892/etm.2020.8671. Epub 2020 Apr 22. PMID: 32509006; PMCID: PMC7271730.
- Novotný JS, Gonzalez-Rivas JP, Kunzová Š, Skladaná M, Pospíšilová A, Polcrová A, Medina-Inojosa JR, Lopez-Jimenez F, Geda YE, Stokin GB. Risk Factors Underlying COVID-19 Lockdown-Induced Mental Distress. Front Psychiatry. 2020 Dec 21;11:603014. doi: 10.3389/fpsyt.2020.603014. PMID: 33424666; PMCID: PMC7793642.
- Akkaya-Kalayci T, Kothgassner OD, Wenzel T, Goreis A, Chen A, Ceri V, Özlü-Erkilic Z. The Impact of the COVID-19 Pandemic on Mental Health and Psychological Well-Being of Young People Living in Austria and Turkey: A Multicenter Study. Int J Environ Res Public Health. 2020 Dec 6;17(23):9111. doi: 10.3390/ijerph17239111. PMID: 33291276; PMCID: PMC7730981.
- Singh S, Bedi D. Financial Disruption and Psychological Underpinning During COVID-19: A Review and Research Agenda. Front Psychol. 2022 Jul 14;13:878706. doi: 10.3389/fpsyg.2022.878706. PMID: 35910967; PMCID: PMC9333085.
- Swift HJ, Vauclair CM, Abrams D, Bratt C, Marques S, Lima ML. Revisiting the paradox of well-being: the importance of national context. J Gerontol B Psychol Sci Soc Sci. 2014 Nov;69(6):920-9. doi: 10.1093/geronb/gbu011. Epub 2014 Feb 24. PMID: 24567313.
- Otten D, Tibubos AN, Schomerus G, Brähler E, Binder H, Kruse J, Ladwig KH, Wild PS, Grabe HJ, Beutel ME. Similarities and Differences of Mental Health in Women and Men: A Systematic Review of Findings in Three Large German Cohorts. Front Public Health. 2021 Feb 5;9:553071. doi: 10.3389/fpubh.2021.553071. PMID: 33614574; PMCID: PMC7892592.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
